This Year's Healthcare Economic Winners
and Losers, and Issue With the Greatest Impact
This week, MCOL released results of the annual
survey of healthcare stakeholders held in
conjunction with the Future Care Web Summit, on
which key topic would have the greatest impact,
and what stakeholders would be economic winners
and losers during this year.
Participants were asked to respond to three
items:
1. Which one of these six topics will
have the greatest impact on stakeholders in
2022?
- Regulatory Health Policy
Changes
- Continued Growth in
Telehealth
- Continued Provider
Economic Losses Resulting from Pandemic
- Increased Utilization/ Negative Outcomes from
Prior Deferred Care
- Provider
Staffing Issues Due to Pandemic/Burnout
- Other Issues
2. Please project who you
think the economic winners and losers for 2022
will be. Who do you think will be economically
better off, the same or worse off by this time
next year: Consumers; Employers; Health Plans;
Hospitals; Physicians; Pharmaceutical
3.
Please indicate your perspective:
Purchaser (Health Plan, Employer, TPA, Agent,
PBM); Provider (Hospital, Physician,
Pharmaceutical, Other Providers); and Vendor or
Other
Stakeholders overwhelmingly
selected “Provider Staffing Issues Due to
Pandemic/Burnout” (49.0%) as the topic having
the greatest impact in 2021, followed by
“Regulatory Health Policy Changes” (17.6%).
Last year – in 2021- 38.2% selected Biden
Regulatory Health Policy Changes, followed by
17.1% for Increased Utilization/ Negative
Outcomes from Prior Deferred Care.
Providers, Purchasers, and Vendors/Others were
relatively equal in naming provider staffing
issues as the highest impact topic, with 52.4%,
50.0% and 46.2% doing so respectively. However,
responses by these categories differed in which
topic followed in being named the highest
impact, with Providers and Purchases listing
Regulatory Health Policy Changes (23.8% and
25.0% respectively) and Vendors/Others naming
Continued Growth in Telehealth (15.4%.)
When ranking these six topics, with 1 being the
highest impact and 6 being the lowest (and only
assigning each number to one topic), Provider
Staffing had the lowest average number ranking
(indicating greatest impact) with 2.41. The
other four specified topics ranged from 3.10 to
3.71, while all “Other Issues” averaged 4.82.
Pharmaceutical was again named the biggest
economic winner for 2022 (56.0% said they would
be better off, compared to 68.4% last year) and
was the only category with greater than 50%
indicating so (Health Plans came in second at
45.1%, and all other categories ranged from
11.8% to 17.6%.).
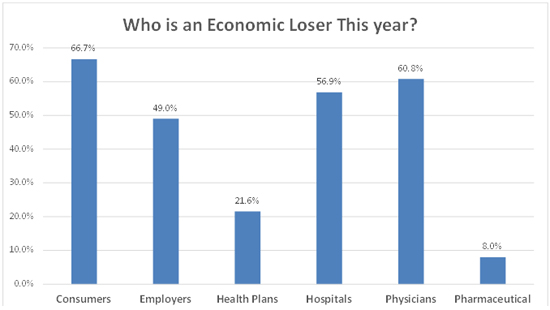
With respect to losers
this year – Consumers again came out on bottom
(66.7% for 2022 and 63.2% in 2021) while
Pharmaceutical again reflected the least
pessimism (8.0% this year and 10.5% in 2021
picked them as losers.)
While zero
percent of Providers Physicians as Better Off in
2022 (compared to 11.8% overall), more
Vendors/Others actually picked them to be worse
off (65.4% said Physicians would be worse off,
compared to 57.1% of Providers.) More
Vendors/Others also felt Hospitals would be
worse off, compared to Providers (69.2% vs.
47.6%).
For
Mor
e Information:
Future Care Web Summit 2022
https://healthexecstore.com/products/webinar-future-care-web-summit-2022